Hope Programme in Neighbourhood Health Service: Community-led self-management for patient activation
“Neighbourhood health aims to create healthier communities, helping people of all ages live healthy, active and independent lives for as long as possible while improving their experience of health and social care, and increasing their agency in managing their own care.”
Across every neighbourhood in England, long-term conditions are now the norm rather than the exception. 1 in 4 of us already lives with at least one long-term condition, and many juggle two or more alongside work, caring responsibilities and the everyday business of life. At the same time, demand on the NHS continues to rise: emergency admissions have increased by more than 40% over the past decade, with over 60% of emergency inpatients now living with at least one long-term condition.
Why patient activation matters
People with long‑term conditions spend under 1% of their time in contact with health professionals; the remaining 99% of care is self‑management, often supported informally by family and communities. Patient activation – a person’s knowledge, skills and confidence to manage their health – is a powerful predictor of how that self‑management plays out in practice. Research using the Patient Activation Measure (PAM) shows that, compared with those least able to self‑manage, highly activated patients have around 38% fewer emergency admissions, 32% fewer A&E attendances, and 18% fewer GP appointments. At population level, analysis from the Health Foundation suggests that if people with the lowest activation were supported even one level upwards, this could prevent hundreds of thousands of emergency admissions and A&E attendances each year.
Supported self-management as core business
NHS England positions supported self‑management as a core component of the Comprehensive Model for Personalised Care, alongside shared decision making, social prescribing and personal health budgets. Good supported self‑management means systematically helping people build the capabilities to live well with long‑term conditions through health coaching, structured education and peer support, tailored to their level of activation. Evidence from national programmes shows that when people with long‑term conditions receive this kind of support, they report better quality of life, improved mental wellbeing and fewer episodes of unplanned and emergency care. For neighbourhood teams, this is directly aligned with the ambition to shift from reactive crisis care to proactive, community‑anchored support.
The Hope Programme: neighbourhood-ready self-management
Neighbourhood health needs community-led evidence-based solutions. Our Hope Programme has been co-designed with people living with long-term conditions and carers, and is built on decades of research from Coventry University. The programme brings together positive psychology, mindfulness and cognitive behavioural therapy in 6–8 session courses that can be delivered digitally at scale or in local groups, with facilitation by trained staff or peers who often have lived experience. More than 33,000 people have benefited from Hope across the UK to date and published evaluations show meaningful improvements in patient activation, mental wellbeing, quality of life and reductions in depression and anxiety.
HOPE offers one universal solution – built and driven by what people with long-term conditions told us they want - choice, control and focus on “what matters to me”. HOPE is about the person - not their condition. HOPE is about living well - for anybody with long‑term conditions, looking after someone, feeling lonely, isolated, anxious or depressed. HOPE is holistic - it helps people reflect, start where they are, focus on what they can do rather than what they can’t. It’s about meeting others, sharing and learning practical tools to manage symptoms, deal with setbacks, have healthier lifestyles and re-discovering their strengths. It helps people set realistic personal goals and be more confident when communicating with health professionals to get the most out of their care. HOPE is flexible in delivery - with options for quality assured digital or in‑person courses, and ongoing peer-support and events through our community.
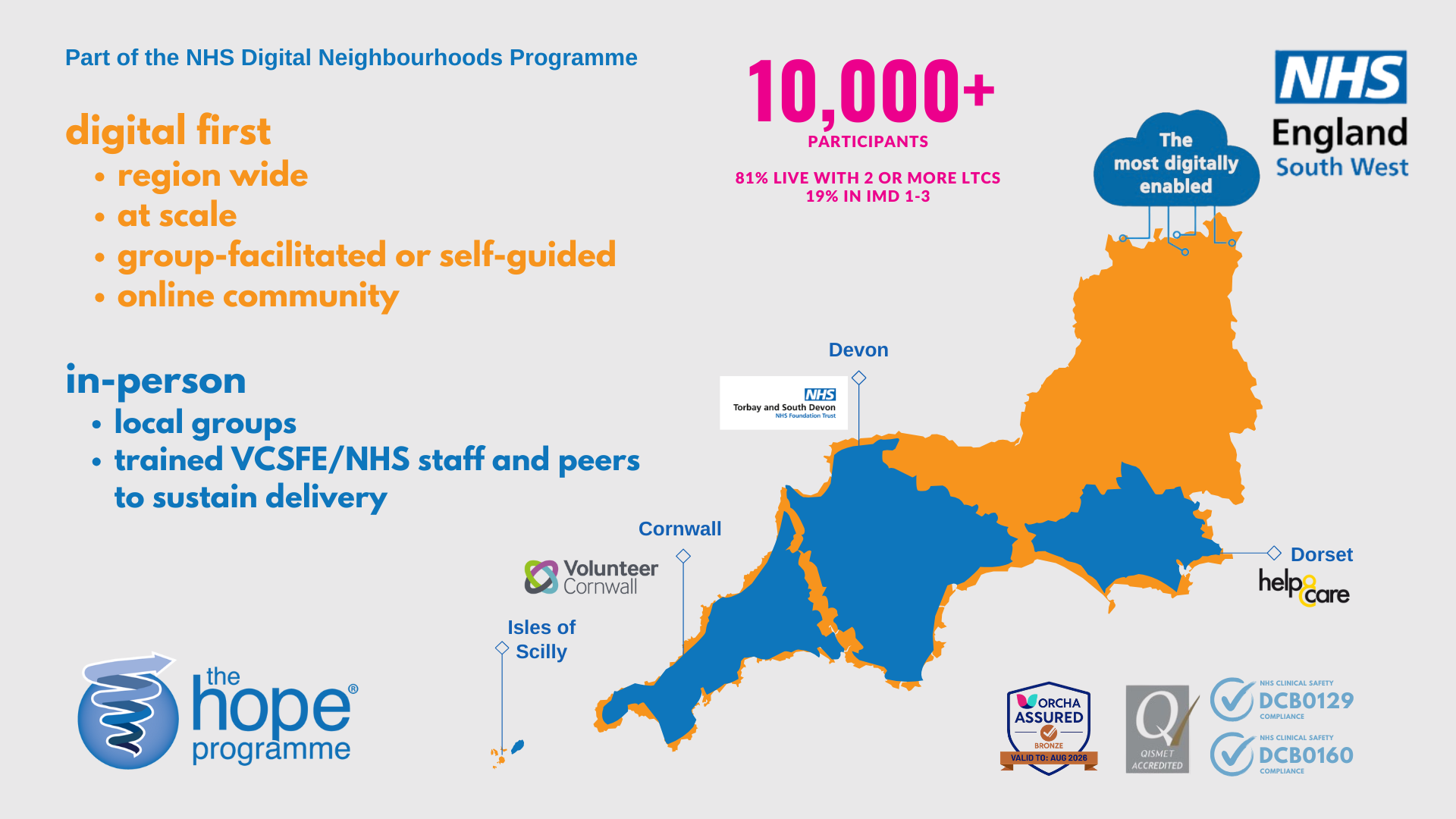
Hope is delivered in partnership with the NHS, public and impact sector organisations. In the South West of England, part of the NHS Digital Neighbourhoods Programme, Hope is being offered to 10,000 people across the whole region as a “digital-first” self-management offer, underpinned by clinical safety approval and complemented by in-person groups run in Dorset, Devon and Cornwall for those with low digital confidence.
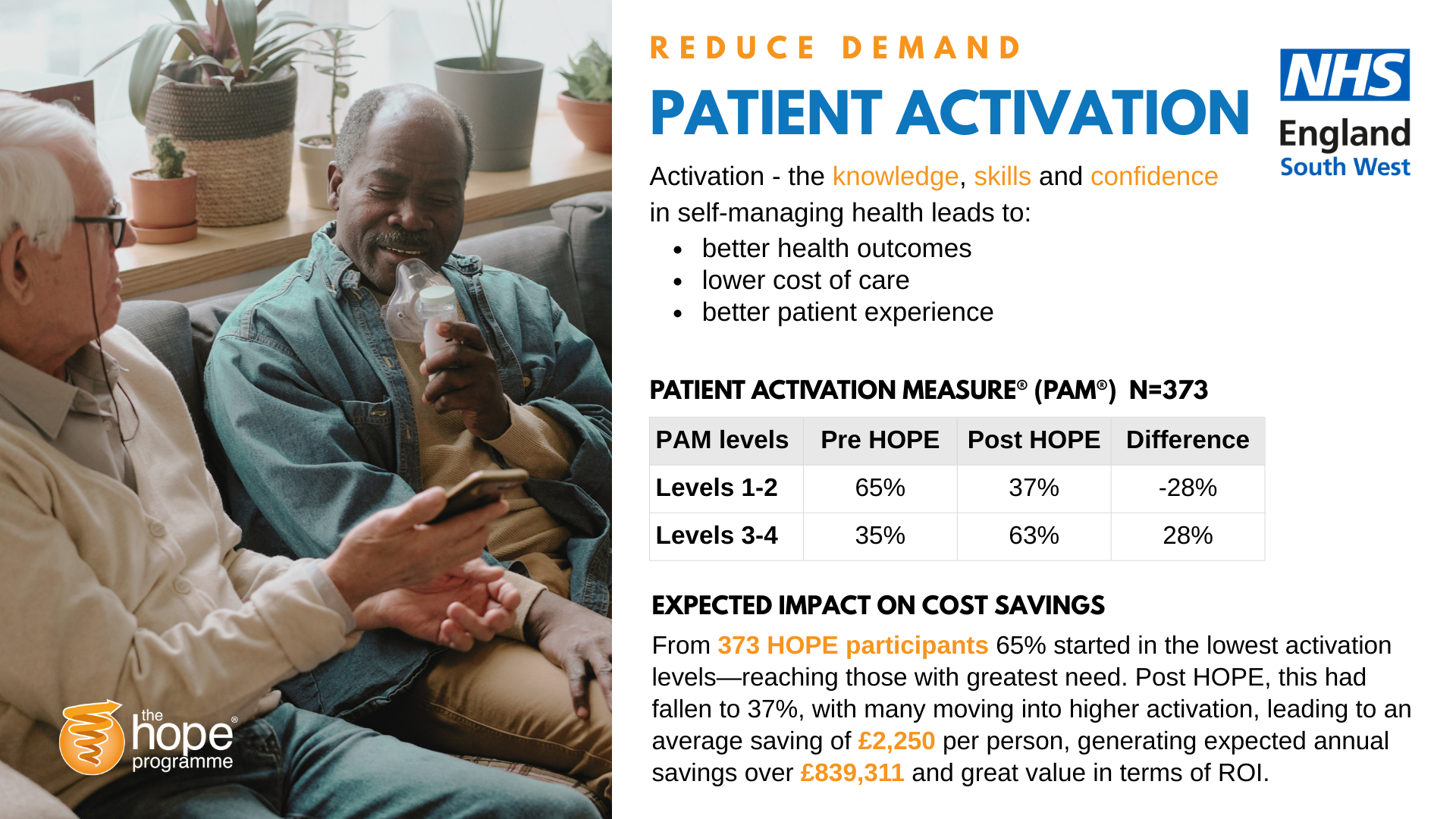
Real-world evaluation using PAM data from 373 participants on the digital Hope Programme show that almost two-thirds started in the lowest activation levels, yet by course end this had fallen to 37%, with many people moving into higher activation levels associated in the literature with lower utilisation and less “wasteful” use of care. Modelling from Barker et al. in BMJ Quality & Safety and the Health Foundation suggests that such shifts in activation correspond to substantial reductions in emergency care use and average health‑care costs per person per year across a whole health economy.
Hope Programme offer in the South West of England
Patient activation data analysis and savings using Phreesia PAM
How the Hope Programme supports the six core components of neighbourhood health:
Modern general practice – Offers GPs and practice teams a structured, evidence‑based self‑management course they can sign-post to via social prescribing or personalised care roles, reducing repeat appointments and supporting people between contacts.
Neighbourhood multidisciplinary teams (MDTs) – Provides MDTs with a shared activation‑building pathway for people with multiple physical and mental health needs, including those who do not fit single‑condition pathways, and generates PAM data that can inform shared care planning.
Integrated intermediate care with a “home first” approach – Helps people rebuild confidence, manage symptoms and prevent relapse after a crisis, hospital stay or step‑down from intermediate care, supporting safe discharge and recovery at home
Secondary care contribution to neighbourhood health – Gives hospital teams a practical self‑management offer to “hand back” to neighbourhood services (for example, after surgery, cancer treatment or long COVID clinics), reinforcing prevention and supported recovery beyond the hospital walls.
Community health, mental health and social care services – Wraps around existing community and mental health provision, adding peer support, digital tools and skills‑building that help people manage day‑to‑day life with long‑term conditions and co‑existing anxiety or low mental health.
Population health management and reducing inequalities – Targets and tracks improvements in knowledge, skills and confidence (using measures like PAM), focusing on people with multiple conditions, low activation and higher deprivation, where the potential to reduce avoidable use and narrow inequalities is greatest.
Building neighbourhood health, not just delivering courses
For neighbourhood multidisciplinary teams, Hope offers a flexible option that can be embedded across pathways – from “waiting well”, mental health and multi-morbidity. Because the course is condition-agnostic and modular, it can be rapidly adapted to local priorities while avoiding the duplication and cost of multiple single-condition apps. This aligns with calls from national reports to rationalise digital self-management offers and invest instead in a small number of robust platforms that can meet the needs of many. Critically, Hope does not stop after one course, it includes peer-support and ongoing access to resources in Hope community which are central to sustained activation and to reducing health inequalities in communities facing deprivation.
Neighbourhood health is ultimately about shifting power – enabling people and communities to do more of what keeps them well, and using finite NHS resources where they add most value. The evidence on supported self-management and PAM shows that investing in activation is not a ‘nice to have’: it is a practical route to fewer avoidable admissions, better experiences and better use of the public funds.
Time‑limited opportunity to test Hope: Neighbourhood Health Innovation Fund
On Thursday 22 January 2026, 13:00–14:30, Grow Digital Health Midlands hosted a virtual Neighbourhood Health Innovation Showcase, launching the Neighbourhood Health Innovation Fund offering awards of up to £20,000 to help Midlands health systems implement digital technologies that enable a neighbourhood health model.
If you are part of an Integrated Neighbourhood Team, a Primary Care Network, a trust, ICB or local authority, this is an opportunity to explore how the Hope Programme could support your neighbourhood priorities.